Whether the need results from a traumatic fracture or surgery to remove a cancerous tumor, decisions about how to restore bone in patients can have a lasting impact on their ultimate recovery.
In treating such defects in the skull, upper jaw, lower jaw or orbital bone — the eye socket — regenerating bone often is done in one of two ways.
There’s autologous bone grafting, in which a patient’s own bone is taken from another part of the body and used to stimulate growth in the injured area. It’s not ironclad, though, as implant morbidity is still a present reality, not to mention the toll multiple surgeries can take on a patient.
“If the technology works as anticipated, it will revolutionize the reconstruction of such complex three-dimensional structures. Reconstruction of such complex facial bony defects would become less of an art and more of a science.”
—Dr. Likith Reddy
Another option is grafting synthetic materials to stimulate bone healing; however, timing is a problem. From the time of injury or surgery to the generation and delivery of the material — FDA-approved calcium phosphates, titanium metal and suture-grade polymers — there is a critical wait period of three to four weeks. It’s time a patient simply does not have if bone is to heal properly.
“Sometimes you’ll have a traumatic fracture injury; the bone will break, and then it will continue to resorb into a defect. In some cases these can involve craniofacial defects in a non-load bearing area, like the skull,” says Dr. Venu Varanasi, assistant professor in biomedical sciences.
A new technology from Varanasi and Texas A&M College of Dentistry researchers could stand to revolutionize the treatment process, giving medical professionals another option for healing bone, and a significantly faster one at that.
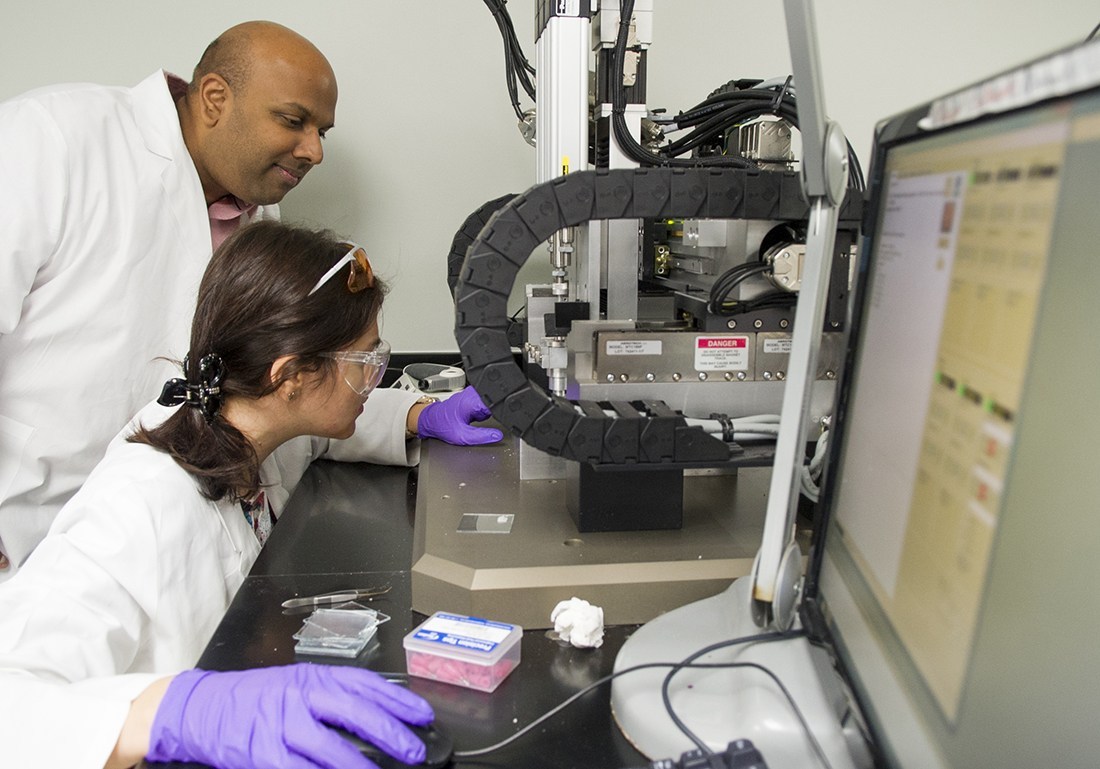
It’s called 3-D live printing, a process in which substances such as bioactive biopolymers are integrated with bioceramic materials and literally printed onto the affected area, forming a scaffolding rich in blood, and with it, oxygen, for new bone to grow.
“Our bioceramics are biodegradable, or they can be engulfed through cells,” Varanasi explains. “The intent in the end is to rapidly deliver the therapeutic, induce the healing at an earlier point, and then allow the cells and the tissue to overtake the material, consume the material, and allow for full restoration of natural bone.”

Coordinates for the 3-D printer can be customized to fit the necessary scaffolding size and printed directly onto the bone.
It’s a concept that has generated promising results since testing began on animal models in spring 2015. To date, the chemical makeup of the new bone has been found to be comparable to the bone surrounding the defect. Current National Institutes of Health – National Institute of Dental and Craniofacial Research funding dating back to 2014 as well as Texas A&M University intramural grants have made these efforts possible.
Researchers in Varanasi’s lab are fine-tuning the methodology and can now complete the entire printing process within 45 minutes. The object here is scale-ability, ensuring the process can be replicated in a hospital operating room. It doesn’t hurt that heading up testing are University of Texas at Arlington collaborators Dr. Felipe Monte, an orthopedic surgeon and doctoral candidate, and Tugba Cebe, a graduate student.
Successful outcomes for 3-D bone printing could give oral and maxillofacial surgeons an additional option for reconstructing facial defects, whether they occur as a result of trauma, congenital defects or pathology, says Dr. Likith Reddy, associate professor in oral and maxillofacial surgery and director of residency training.
“The gold standard for reconstruction of such defects involves carving of the cranial bone, hip bone or the leg bone to recreate the missing structures,” Reddy says. “This is technically impossible for large facial defects.”
Additional technology utilizing alloplastic materials to recreate the missing facial elements is another current treatment method but not without its drawbacks.
“This requires about three to four weeks of waiting at a minimum,” Reddy adds. “In addition, if we need to change anything during surgery, this preplanned and printed construct is of no use.
“The in vivo printing technique will attempt to solve both the problems. If the technology works as anticipated, it will revolutionize the reconstruction of such complex three-dimensional structures. Reconstruction of such complex facial bony defects would become less of an art and more of a science.”
The developing technology also holds the potential for substantial strides in a patient’s total rehabilitation and well-being, such as with facial prosthetic reconstruction.
“By combining the expertise of our colleagues in biomedical sciences within the bioengineering core, there is a future of possibly creating a bioengineered prosthesis, rebuilding the anatomy with a ‘bio-active’ material,” says Suzanne Verma, anaplastologist and assistant professor in oral and maxillofacial surgery at the dental school.
By contrast, current facial prostheses are fabricated from silicone rubber and retained to the face with an osseointegrated implant-and-magnet system.
“By working together and introducing bioengineering principles and tools into the workflow, the clinical process is transformed,” Verma adds.
To help such collaborations advance to that next level, Varanasi and the Texas A&M Office of Technology Commercialization have been in talks with potential investors. Proposals for commercialization and scientific research grants with National Institutes of Health, National Science Foundation, the Department of Defense, and collaborations with industry will be pursued.
Meanwhile, College of Dentistry researchers will continue to develop the technology to enhance reproducibility.
Depending on outcomes, Varanasi’s hope is to apply 3-D printing to other parts of the body as well.
“That’s the holy grail,” Varanasi says. “You can just take off-the-shelf components in the OR, print them directly into the bone defect, and the patient’s own bone is doing the healing. There are a lot of possibilities. That’s the beautiful thing about it.”